A case-control study of cerebellar tonsillar ectopia (Chiari) and head/neck trauma (whiplash)
Freeman Michael D. et al. Brain Injury, July 2010; 24(7-8):988-994
Many in the in Upper Cervical circles are familiar with Dr. Scott Rosa and his collaborative effort on cerebellar tonsillar ectopia (CTE), and for those of you who are not familiar this is a powerful article for any doctor’s knowledge on the effects of whiplash trauma and the brain stem.
Study: This was a case-control study where cervical MRI scans of 1200 neck pain patients were reviewed. 600 of the cases had a history of trauma, 600 cases where controls (non-trauma). Half the cases where scanned in an upright MRI, half in a recumbent position. Two radiologists looked at each study for the level of the cerebellar tonsils.
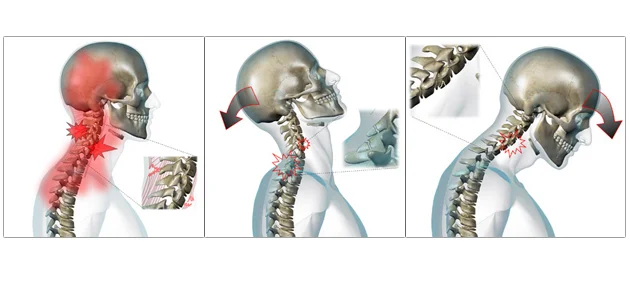
Whiplash is a series of movement with first compression forces, then hyper-extension, and then hyper-flexion. The most commonly damaged structures are ligaments.
Results: The study reports that patients with a history of motor vehicle crash-associated neck pain have a substantially higher frequency of cerebellar tonsillar ectopia of 1mm or more than non-traumatic subjects.
Clinical Pearls: Symptoms associated with CTE are occipital headache, neck pain, upper extremity numbness, paresthesias and weakness, and in rare cases lower extremity weakness and signs of cerebellar dysfunction.
Neuroradiographic diagnosis is positive when the cerebellar tonsils descend 2 or more millimeters below the basion-opisthion line (foremen magnum)
CTE among the trauma group was noted 2.5 times more in upright MRI studies than in recumbent MRI studies and 4 times more often than in either of the non-traumatic controls. Gravity dependent instability may exist with traumatic cases and should be evaluated in an upright position if possible.