Follow-Up MR Imaging of the Alar and Transverse Ligaments after Whiplash Injury:
A Prospective Controlled Study
Vetti N., Krakenes J. et al. American Journal of Neuroradiology 32: 1836-41, Nov 2011
Why do we do research? To answer questions? Yet, how often do we seek out research that validates our paradigm? My guess would be almost always. Therein is the problem. To be a true question, we must not think we already know the answer or outcome. That was the reason that this study caught my eye.
This study was a prospective case controlled study that followed 91 symptomatic whiplash patients and 52 neck pain control patients for 1 year. MR Imaging was done at baseline on neck pain patients and after the accident and on a 1 year follow up, results were also correlated with the neck disability index.
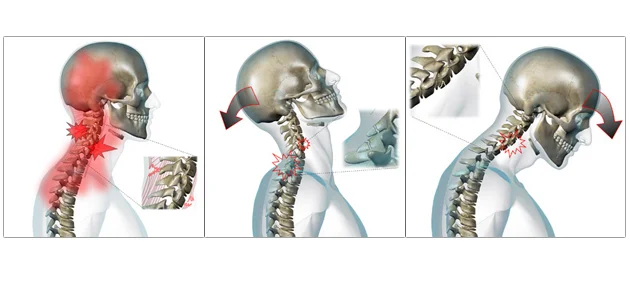
The inclusion criteria for the whiplash included: MVA in the past 7 days with onset of neck pain within 48 hours. No previous history of neck pain, and classified as WAD 1-2 (Whiplash Associated Disorders without any neurological signs, factures or dislocations).
The symptomatic control patients were included when they reported to an outpatient spine clinic with a history >3 months of neck pain with a non-traumatic onset.
The researchers concluded that the areas of high signal intensity (indicating inflammation/fibrosis/fat replacement) in the alar and transverse ligaments did not change significantly at baseline or at 1 year follow up for WAD patients. Further the prevalence of the alar and transverse ligament high signal intensity did not differ significantly between traumatic and non-injured neck pain controls.
What the researchers concluded is that the alar and transverse ligament high signal intensity in patients with WAD1-2 observed in the first year after injury cannot be explained by the trauma.
Clinical Pearls:
“High signal intensity could theoretically be due to altered ligament function cause by neck pain.”
“Pain induced immobility causes morphologic changes in muscles, tendons and ligaments.”
“High signal intensity of the alar and transverse ligaments is also reported to be frequent in healthy non-injured persons without neck pain.”
Author’s Note: This study is a bit confounding however provides an interesting observation on neck pain related MR imaging.