Migraines are more than just bad headaches, as sufferers know all too well. So if you’ve been experiencing severe headaches, how can you know if this is actually a symptom of a migraine? Here are some more symptoms of migraines. Remember that people often exhibit different symptoms, so you may have some that are not listed here, but these are a few of the more common ones.
· Sensitivity to light, sounds, and/or smells
· Nausea and/or vomiting
· Dizziness or vertigo
· Visual disturbances (possibly including temporary loss of vision)
To learn more about the connection between head and neck injuries and migraines click the image below to request our complimentary e-book.
What Brings on a Migraine?
If your headaches turn out to be migraines, what can you do to prevent attacks, or keep them as far apart as possible? Here are a few practical suggestions:
· Keep a diary – This will allow you to determine if certain foods, beverages, activities, or other triggers precede your attacks and avoid these.
· Decrease stress levels – Migraines are often triggered by stress. You can reduce stress with a hot shower, a massage, some meditation, stretching, enjoying a hobby, or any other stress relief technique you can think of. Just remember to mark it in your journal if the stress relieving technique actually triggers a migraine.
· See an upper cervical chiropractor
Why See an Upper Cervical Chiropractor?
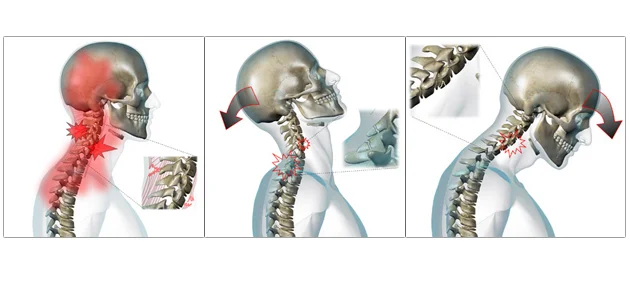
The fact is that your migraines may be the result of an upper neck misalignment. If you’ve ever been in an accident, suffered a sports injury, or even just hit your head, you may have a misalignment of the atlas (C1 vertebra). This isn’t something that would be corrected by a general chiropractor. It involves very specific measurements of the misalignment along with a very precise correction. At Arete Chiropractic, we use the Blair upper cervical technique to deliver just such an adjustment to our patients. In many case studies, upper cervical care has helped individuals suffering from migraines in as few as 1 to 2 adjustments.
To schedule a consultation with Dr. Beebe or Dr. Evans click the button below or call 603-380-9184